This page will give you a brief guide to Sickle Cell Disorders and provide links to more detailed information for different groups of users.
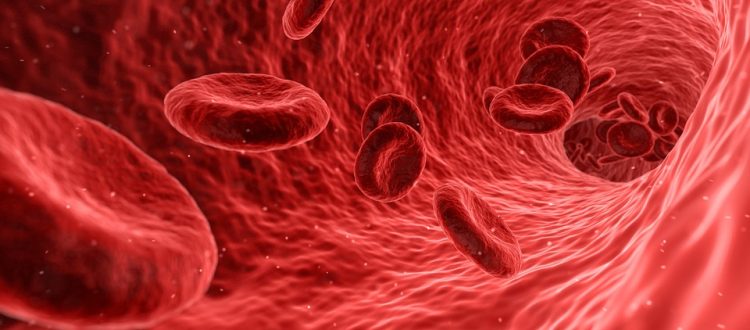
The disorder affects the red blood cells which contain a special protein called haemoglobin (Hb for short). The function of haemoglobin is to carry oxygen from the lungs to all parts of the body.
People with Sickle Cell Anaemia have Sickle haemoglobin (HbS) which is different from the normal haemoglobin (HbA). When sickle haemoglobin gives up its oxygen to the tissues, it sticks together to form long rods inside the red blood cells making these cells rigid and sickle-shaped. Normal red blood cells can bend and flex easily.Blocked blood vessels
Because of their shape, sickled red blood cells can’t squeeze through small blood vessels as easily as the almost donut-shaped normal cells. This can lead to these small blood vessels getting blocked which then stops the oxygen from getting through to where it is needed. This in turn can lead to severe pain and damage to organs.
Everyone has two copies of the gene for haemoglobin; one from their mother and one from their father. If one of these genes carries the instructions to make sickle haemoglobin (HbS) and the other carries the instructions to make normal haemoglobin (HbA) then the person has Sickle Cell Trait and is a carrier of the sickle haemoglobin gene. This means that this person has enough normal haemoglobin in their red blood cells to keep the cells flexible and they don’t have the symptoms of the sickle cell disorders. They do however have to be careful when doing things where there is less oxygen than normal such as scuba diving, activities at high altitude and under general anaesthetics.
If both copies of the haemoglobin gene carry instructions to make sickle haemoglobin then this will be the only type of haemoglobin they can make and sickled cells can occur. These people have Sickle Cell Anaemia and can suffer from anaemia and severe pain. These severe attacks are known as Crises. Over time Sickle Cell sufferers can experience damage to organs such as liver, kidney, lungs, heart and spleen. Death can be a result.
Another problem is that red blood cells containing sickle haemoglobin do not live as long as the normal 120 days and this results in a chronic state of anaemia. In spite of this, a person with sickle cell disorder can attend school, college and work. People with sickle cell disorder need regular medical attention particularly before and after operations, dental extraction and during pregnancy. Many hospitals arrange follow-up appointments and it is advisable to discuss with the doctors questions concerning schooling, strenuous exercise, family planning, suitable types of employment and air travel. When a person is found to have a sickle cell disorder it is important that all members of the family be tested. They will not necessarily have sickle cell disorder but may be healthy carriers of a sickle cell trait.
Other types of Sickle Cell Disorders (SCDs)
There are also other different types of haemoglobin such as HbC and beta thalassaemia, that can combine with sickle haemoglobin to cause sickling disorders. When someone carries the gene for beta-thalassaemia they cannot make as much HbA as they should. If this is combined with the HbS gene then more of their total amount of haemoglobin is HbS and they can suffer from what is usually a milder form of sickle cell disorder than sickle cell anaemia.
Who Gets SCDs?
The different kinds of SCD and the different traits are found mainly in people whose families come from Africa, the Caribbean, the Eastern Mediterranean, Middle East and Asia.* In Britain SCD is most common in people of African and Caribbean descent. It is estimated there are more than 15,000 adults and children with SCD in Britain at present. Every year about 350 babies are born with SCD. There are other inherited conditions that mainly affect other groups, e.g. Cystic Fibrosis in Europeans, and Tay-Sachs disease in Jewish people.
Testing for SCDs
A special blood test (haemoglobin electrophoresis) can tell you whether you have a sickle cell disorder or are a healthy carrier, e.g. for sickle cell trait. Routine screening should take place for all pregnant women, all newborn babies, and before anaesthesia, either at hospital or dental clinics.
Tests for pregnant women are offered by midwives. This test should be offered before 10 weeks of pregnancy. A test is offered to the baby’s father if the woman is found to be a carrier for sickle cell disease. If both parents are carriers of SCD the unborn child can be tested from 11 weeks of pregnancy to see if it has SCD. For more information see the Prenatal Testing page and contact your local sickle cell centre, local obstetrician, haematologist or general practitioner.
Tests can also be arranged by your general practitioner or at our local sickle cell centre. (Contact us for an up-to-date list of centres in the UK.) After a blood test you may be told that you or your child is `sickle positive’ or has `sickle cell’. It is important to ask whether this means sickle cell trait or a type of sickle cell disorder.
What Sickle Cell Disorders are Not
People are often confused and disturbed by some of the incorrect information they have received about SCD.
Sickle Cell Disorders
are not leukaemia
are not cancer
are not white blood cells eating up red blood cells
are not infectious – you cannot `catch it’ as you would catch measles or a cold.
Sickle Cell Disorder is a condition which is inherited from both parents. This means that people are born with it, just as they are born with other characteristics such as eye colour, hair texture and height.
For further information contact:
Sickle Cell Society
54 Station Road
London, NW10 4UA
UK
Tel 020 8961 7795
Fax 020 8961 8346
info@sicklecellsociety.org